

SPRAVATO® Payer Coverage Considerations
Learn more about how payer policies may impact patients’ access to treatment and determine the appropriate acquisition method.


Learn more about how payer policies may impact patients’ access to treatment and determine the appropriate acquisition method.
Review the following considerations for navigating payer requirements, contract negotiations, and patient coverage:

Get a full view of your patients’ insurance coverage, including insurance type (eg, commercial, Medicare, Medicaid) and payer benefit design (medical and/or pharmacy) to understand the preferred pathway and help patients start treatment quickly

Once a prescribing decision has been made, SPRAVATO withMe can help navigate access and affordability processes efficiently so you can focus on your patients

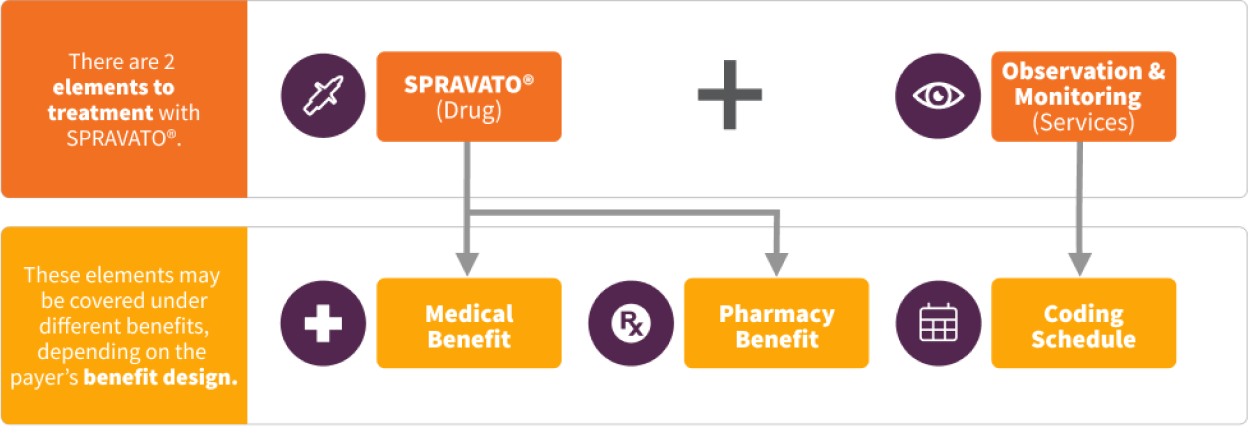
When determining how you will acquire SPRAVATO®, consider contacting your payers to understand how SPRAVATO® (drug) and observation and monitoring (services) are covered in your payer policies

Establishing transparent payer contracts can help facilitate patient access to treatment. Consider key points such as the payer’s preferred acquisition method, prior authorization criteria, and reimbursement time frames when discussing terms
If you are experiencing access challenges, consider working with payers to understand their policies. Ask if your patient’s insurance plan uses a behavioral health organization (BHO). If so, contact the BHO to understand your reimbursement and coding options.
Exception: If the benefits investigation determines that SPRAVATO® is subject to restrictions or not covered, consider submitting a medical exception request to the patient’s health plan. Access a sample Letter of Exception template.
Appeal: If a PA or medical exception request is denied for clinical reasons, consider submitting an appeal request to the patient’s health plan. Access a sample Letter of Medical Necessity template.
Patient access to SPRAVATO® improves through the use of both medical and pharmacy benefits. Check with your patient’s insurance plan to understand which pathway is preferred.
PA=prior authorization; REMS=Risk Evaluation and Mitigation Strategy.